Learning how to prepare for a contraception appointment can help you feel empowered when accessing contraception and find the method that’s right for you. In this blog, MSI UK’s Kayla Healey (Registered Midwife and Faculty Registered Trainer) and Tanya Lane (Registered Nurse and Faculty Registered Trainer) share some top tips on how to prepare for a contraception appointment, including:
- What to consider before your contraception appointment when choosing a method that suits you
- What to ask during your contraception appointment
- What to expect after your appointment, and what to do if you want to change your method of contraception
What to consider before your contraception appointment?
There are a range of contraception methods available, and when it comes to deciding which to use, it’s not a one-size-fits-all approach.
All methods will be discussed during your appointment with a clinician, but there are a few things you might want to consider ahead of your appointment to help you choose the best option for you.
Short-acting or long-acting contraception?
One important thing to consider when thinking about contraception is whether you’d prefer a method that you don’t have to remember or think about taking and replacing, or whether you’re happy to take and replace your method more regularly.
If you are happy to take contraception more regularly or every day, you may wish to start with a short-acting method of contraception like a contraceptive pill, the contraceptive patch and the contraceptive ring. The appropriateness of some of these methods – such as whether the combined pill or the progestogen-only (mini) pill is best for you – will depend on your medical history, which would be checked during your appointment. If you’d like to use a short-acting method of contraception but don’t think you’ll be able to take a pill at the same time each day, the patch or the ring might be a good alternative (as they have to be replaced less often).
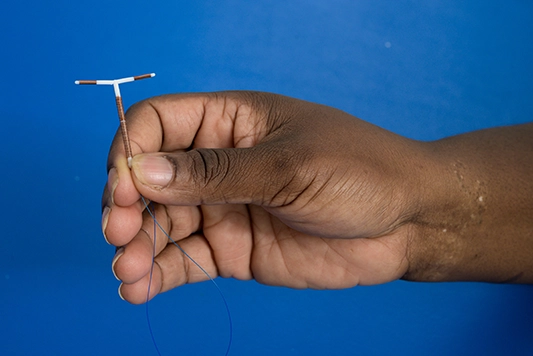
If you would rather not have to remember to take contraception every day and know that you do not want to get pregnant for a while, LARC (Long-Acting Reversible Contraception) methods (also known as fit-and-forget methods) might be best for you. These include the IUD (copper or non-hormonal coil), the IUS (hormonal coil), the contraceptive injection and the contraceptive implant.
How might contraception affect your periods?
Another important thing to consider when thinking about your contraceptive options are your periods. Different contraceptive methods can impact your period in different ways, so you may be asked questions like: Are your periods manageable at the moment? Are they painful? Are they heavy? If you have painful or heavy periods, for example, you might want to flag this to the clinician who will advise on methods that can make your periods more manageable (or on methods to avoid). For example, the non-hormonal coil (IUD) may exacerbate heavy or painful periods, whilst the hormonal coil (IUS) or combined contraceptive methods (like the combined pill, the patch and the ring) might be recommended to support with heavy periods.
The combined pill gives you the option to skip or shorten your period. To skip your period, you can continue to take the next pack of pills when you finish your current pack. It’s important to know that not having a regular period as a result of contraception does not cause any harm, and is not a problem for you or your future fertility.
In addition to a potential impact on your periods, there are other non-contraceptive benefits to some contraceptive methods. For example, certain brands of the combined pill can help with acne – a clinician will be able to advise which brand is best for this.
Research has also previously found that combined hormonal contraception is associated with a significant decrease in the risk of endometrial and ovarian cancer, across lifestyle factors. To read more about this, you can read our blog: Contraception, cancer and choice: what are the facts?
How effective are different methods of contraception?
You may also want to consider the efficacy or effectiveness of each method at preventing pregnancy when choosing a contraceptive method. Each method has different rates of efficacy. You can find the efficacy of each method (both with ‘perfect use’ and ‘typical use’) on our long-acting reversible contraception and our short-acting contraception pages.
Hormonal contraception or non-hormonal contraception?
Different contraceptive methods can impact your hormones in different ways. The side effects of some hormonal contraceptive methods may include headaches, nausea, breast tenderness and mood changes.
If you’d prefer to use an entirely non-hormonal method of contraception, condoms or the non-hormonal coil (IUD) may be a good option for you.
Whilst the IUS (hormonal coil) releases a hormone called progesterone, this hormone is localised, and so it is less likely that you’ll experience the same sorts of side effects associated with combined contraceptive methods like the combined pill, patch or ring. Additionally, there are different doses of hormones in different types of IUS – for example, the Mirena coil and Levosert has a higher dose than the Kyleena coil.
Everyone’s experience is different and valid. If you feel like your contraceptive method is affecting you negatively, providers will be able to discuss an alternative with you.
During your contraception appointment: what to expect and what to ask
What to expect during a contraception appointment
During a contraception appointment, a clinician will explore and explain all of your options. This is a chance for you to discuss any specific needs or desires from contraception – for example, if you would like a method of contraception that can support with things like heavy periods or acne.
The clinician may ask you some safeguarding questions, as this is common practice. You may also want to consider having an STI test during your appointment – particularly if you are having a coil fitted.
If, during your contraception appointment, you decide you’d like to start a short-acting method (such as contraceptive pills, the patch or the ring), you will either be given these methods there and then (if you go to a sexual health clinic) or given a prescription to pick up these methods at a pharmacy (if you go to a GP).
Coil fitting and pain management
As with many aspects of contraception, the experience of having intrauterine contraception (such as the hormonal coil or non-hormonal coil) fitted differs from person to person.
The most important thing to remember is that you can ask for pain relief. At MSI Reproductive Choices, we offer anyone opting for a coil a choice of four types of local anaesthetic, including: an anaesthetic gel, spray, an injection and a cream, as well as suggesting the option of taking painkillers, such as ibuprofen, an hour or two before the procedure. Each of these methods of anaesthetic are applied to the cervix (the injection, for example, is applied inside the cervix), and you can choose to have more than one method of anaesthetic if the initial method you use isn’t easing your pain. There is no recovery time for this anaesthetic, and so it is safe for you to drive after your appointment. If you are having your coil fitted or removed with another provider, you may want to ask whether pain relief is provided when you book your appointment.
These anaesthetics may not completely take away the discomfort, and there may still be cramping pain after the fitting (this may last for up to a couple of days).
It’s always good to have something to eat before a coil fitting appointment in case you feel faint at any point, and to wear clothes that are comfortable and easy to change in or out of.
Remember that you are in control, and that you can stop or take a break at any point if you want to. You can also ask to have a chaperone or another healthcare practitioner with you during your appointment, to support you and ensure you feel comfortable throughout.
Contraception recovery and aftercare
How quickly is contraception effective at preventing a pregnancy?
An IUD (non-hormonal coil) is always effective immediately.
If you start to take the progestogen-only pill during the first five days of your period, you will be protected against pregnancy immediately. If you start to take it on any other day, you will not be protected against pregnancy until you’ve taken the pill for two days.
If you start any other methods (including the combined pill, the contraceptive ring, the contraceptive patch, the implant, the injection and the IUS) during the first five days of your period, you will be protected against pregnancy immediately. If you take these methods on any other day, you will not be protected against pregnancy until you’ve used them for seven days.
What can I do if I don’t like the contraceptive method I chose?
For all contraception, we recommend waiting three to six months to see if any negative side effects settle down. However, it’s your body and your choice. If you don’t like a method you’ve chosen, please do get in touch with a provider who will arrange for your method to be removed and explore alternatives.
During your appointment, it’s always good to ask what process to follow if you want to have a method removed.

Our top tips
- Think about which method you might want to try ahead of your appointment, considering things like efficacy, your periods or whether you want a method you need to remember to take every day.
- If you’re having a coil or implant fitted or removed, remember that you can ask for pain relief if you want to! You may want to ask whether your provider offers pain relief when booking your appointment.
- Ask your provider what process you should follow if you don’t like the method that you’ve chosen and want to have it removed.
- Remember that some methods take longer to become effective at preventing pregnancy than others, so you might want to consider using additional contraception (such as condoms) until you are protected.
Read more
To learn more about contraception, the different methods and how to prepare for a contraception appointment, click on the links below:
- Short-acting methods of contraception (the combined pill, the mini pill, the ring, the patch, and condoms)
- Long-acting methods of contraception (the hormonal coil or IUS, the non-hormonal coil or IUD, the injection and the implant)
- Contraception misconceptions
To find out more about the range of contraceptive methods available and get advice on which method might be right for you, check out our online contraceptive counsellor, ‘Choice’.
To learn how you can support access to contraception around the world, check out our Contraception: the unfinished revolution campaign.