For Sexual Health Week 2024, we sat down to interview Tanya Lane (Designate Clinical Excellence Lead for Contraception and Sexual Health) and Kayla Healey (Registered Midwife and Faculty Registered Trainer) from our fantastic contraception team. We spoke with them about the link between contraception and sexual health, where you can go for reliable information on contraception, and what people should know about contraception after an abortion.
“All we can do is provide you with reassurance, your options, and then you still may decide that it’s not for you. We’ll always support that decision.”
How does contraception fit into sexual health?
“Contraception gives people the ability to enjoy their sex lives.”
Kayla: Contraception gives people the ability to enjoy their sex lives. It’s also important to note that condoms are the only form of contraception that protect against sexually transmitted infections.
Tanya: Contraception fits into a holistic approach to sexual wellbeing. If you don’t want to get pregnant, or it isn’t safe for you to get pregnant – physically or mentally – contraception allows you to have sex with less chance of pregnancy.
We recognise that not everyone looking for contraception identifies as a woman: everyone has the right to access contraception without judgement and have all of their needs taken into consideration. We will always support you.
Are there any questions you get asked frequently on contraception?
Side Effects
“You can try something, and you don’t have to stick with it if you don’t like it.”
Kayla: Quite often, people will ask if they’re going to experience side effects, for example weight gain. The answer to that would be that the contraceptive injection is the only method of contraception that has been proven to be associated with weight gain. However, weight gain can be a reported side effect from people that take all forms of hormonal contraception, and this is not the case for everyone. As with almost everything to do with the potential side effects of contraception, it is a case of seeing what works best for you. You can try something, and you don’t have to stick with it if you don’t like it.
“Just because a contraceptive causes one person to have a certain side effect, it doesn’t mean you will have the same experience”.
Tanya: I’d agree – a lot of people ask: ‘Am I going to experience side effects?’ or ‘Is this side effect normal?’. Side effects can include weight gain, changes to mood, changes to skin, libido. It can be difficult to establish cause and effect. There’s a lot of information and people sharing their experiences on social media, but just because a contraceptive method causes one person to have a certain side effect, it doesn’t mean you will have the same experience. Often finding a method that works for you is trial and error.
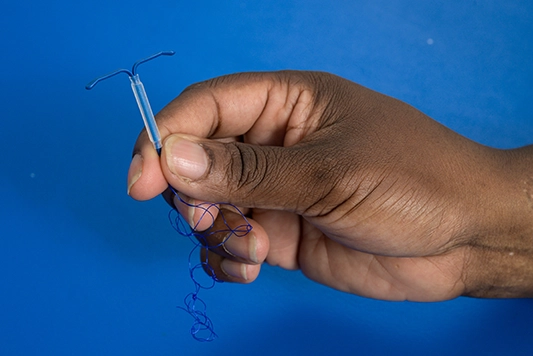
We can also work with a client to find out what would best suit them. For example, I had a client who worked in film and TV, and they were conscious about their skin changing due to contraception. We decided to go down the non-hormonal route with a non-hormonal coil, as this wouldn’t have any impact on their skin.
“Sometimes it can be difficult to advocate for yourself, so we as professionals should be the ones leading the conversation.”
Bleeding
Tanya: Another common question is on what their bleeding pattern will be. This varies method to method, sometimes we will have a definitive answer, and others we will have to give it a go and see.
Coil fitting and pain
Kayla: We also get questions surrounding pain and coil fitting, especially after the recent documentary where Davina McCall got her coil fitted on camera. The experience of pain is going to be different for everyone, but wherever you go, your healthcare professional should offer you pain relief. At MSI UK, we offer pain relief to everyone getting a coil fitted. Sometimes it can be difficult to advocate for yourself, so we as professionals should be the ones leading the conversation.
Do you think people speak enough about contraception?
Kayla: I think everyone will have a different experience. Some schools, for example, will be really excellent at providing this information. It depends what your school is like, if you have a school nurse, what kind of healthcare your GP is interested in, and what type of media you consume (for example, books, news, and social media that discuss contraception).
Sometimes, when speaking to people whilst fitting a coil, I’ll ask them if any of their friends also have the coil. Some people will know exactly what contraception their friends are using, and some people won’t know at all. It really does vary.
Where can people go for reliable information on contraception?
“You want to know what’s going to happen to you when you use a certain form of contraception, and you want to know it from someone with lived experience.”
Tanya: People usually go to social media, or to friends and family for their information. The most valuable, evidence-based information you’ll get would be from sexual health providers, the NHS, MSI UK (for example, our contraception table) and there’s also a really good website called The Lowdown.
Kayla: The reason people are really engaged with social media stories, on TikTok for example, is that you want to know what’s going to happen to you when you use a certain form of contraception, and you want to know it from someone with a lived experience. It feels reliable because it’s coming from someone who probably looks and sounds like you. If you want to hear people’s experiences, I’ll echo Tanya and say that The Lowdown is a really good option.

What would you suggest to someone who is reluctant or nervous to go on contraception?
“We may even be able to suggest something that you’ve not considered before and dispel any myths or misconceptions you may have.”
Tanya: I would start with thinking about what is specifically making you nervous. Is it side effects? Is it the procedure? Then, I would recommend speaking to a healthcare professional about the things you’re nervous about – often we can take a couple off the list of options! We may even be able to suggest something that you’ve not considered before and dispel any myths or misconceptions you may have that are making you nervous.
Kayla: I agree. Uncover what’s making you nervous, and then seek reassurance from a healthcare provider. It’s important to remember that we’re never going to force you into getting something that you don’t want. All we can do is provide you with reassurance, your options, and then you still may decide that it’s not for you. We’ll always support that decision.
What should people know about contraception following an abortion?
“It’s a really convenient time to access contraception.”
Tanya: If you’re not planning to be pregnant again, contraception after an abortion is important, because you can get pregnant very quickly afterwards. It’s a really convenient time to access contraception. At MSI UK, we’re able to provide contraception to six months after you have treatment with us. You can also, of course, visit your local sexual health clinic or local provider for contraception after an abortion.
Some people may be accessing abortion care because their method of contraception failed, and they want to take some time to decide if they want to choose a different method.
“No-one is going to judge you if you decide that you want to leave your abortion appointment without it.”
It’s also important to know that you’re never going to be forced to take contraception. No one is going to judge you if you decide that you want to leave your abortion appointment without it.
Kayla: Our nurses and midwives are trained to have conversations with you about it, so even if they asked you earlier and you didn’t want to talk about it, you can bring it up again at any stage of your treatment.
Tanya: We also understand that not everyone accesses abortion care because they don’t want to be pregnant, for example if you access abortion care to end a pregnancy due to foetal anomaly diagnosis. You may want to become pregnant again soon after.
What do you think are the main challenges facing contraception at the moment?
“It’s so important that there are healthcare professionals, in GP surgeries, in pharmacies, in maternity care, that are knowledgeable.”
Tanya: The conversation on contraception is very open, and this is both a good thing and a challenge. We definitely should be talking about the side effects or risks associated with contraception, but it does open up a space where people can be giving information that isn’t necessarily evidence-based. This is why it’s so important that there are healthcare professionals, in GP surgeries, in pharmacies, in maternity care, that can have these conversations.
Kayla: I think access is the biggest challenge there is. We regularly see people who have had abortions who are on a wait list for contraception elsewhere. Or, clients who are accessing our standalone contraception services* who have been trying to access contraception for months before they get to us.
Tanya: Even if you’ve managed to get through all the information, the decision-making process, you’ve then got to get that appointment. There are cases where someone will want to access a long-acting reversible method of contraception (LARC) but the GP surgery may not have someone that can fit those methods. Additionally, access across the country is going to vary depending on location.
Are there any advancements or changes that you’d like to see in contraception services?
Kayla: For this, my initial reaction is to just say ‘better access’.
“More people being trained, more appointments being available, more investment!”
Tanya: Access to short-term methods is improving. You can access the combined and progesterone-only pills in your pharmacy now, without having to go and see your GP, or visit a sexual health clinic. This is going to be really convenient for some people. Investment in women’s health hubs* should also be a priority and would make a big difference. Also, more people being trained, more appointments being available, more investment in the services.
If you could tell people one thing about contraception, what would it be?
“We hear a lot about the negatives, but there are a lot of positives too!”
Tanya: Contraception can be life changing. It’s empowering. It’s literally changed the world – the reason women can do lots of things now is because they can take control of their reproductive health. You don’t ‘have’ to have children.
Kayla: Contraception can have a lot of benefits outside of just not getting pregnant. For example, the hormonal coil can help with heavy periods, the combined pill reduces the risk of ovarian cancer, and can help with hormonal acne. We hear a lot about the negatives, but there are a lot of positives too!
*In addition to the contraception we offer as part of NHS-funded abortion care, we have a number of clinics across England where we can offer long-acting reversible contraceptive methods (LARC) for people who have not accessed our abortion services. Access to these will depend on the NHS contract that exists in your area.
*Women’s health hubs are a government initiative, aiming to bring together healthcare professionals and existing services to provide integrated women’s health services in the community. This initiative aims to improve access to and experience of care, improve health outcomes, and reduce health inequalities.